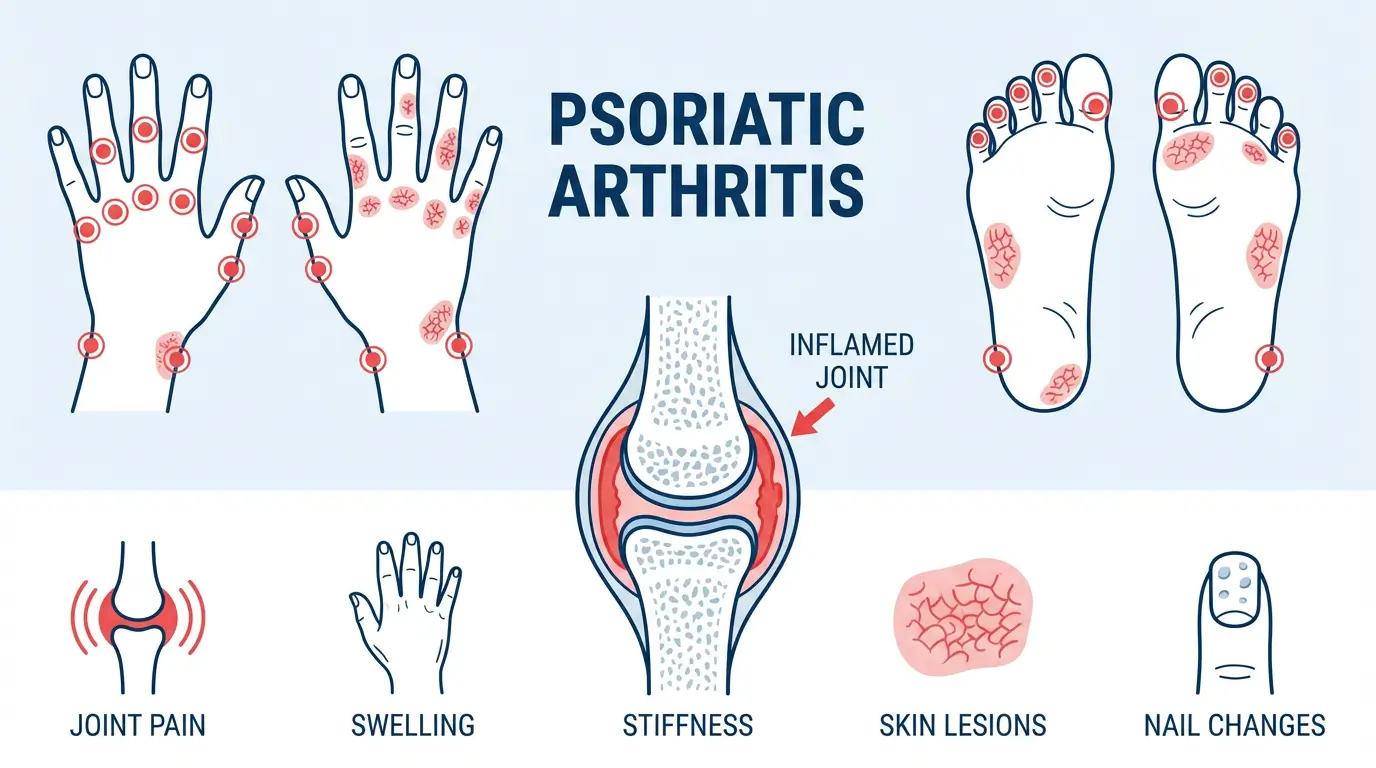
Psoriatic arthritis (PsA) is an autoimmune rheumatic disease and a type of arthritis. It is linked to psoriasis, which is a chronic skin condition. Approximately 7% to 42% of all psoriasis patients also develop PsA (1) at some point in their lives. The most common signs of PsA include joint pain, skin rashes, stiffness, and changes in the appearance of fingernails and toenails.
In this blog, we are going to discuss what psoriatic arthritis is, its symptoms, causes, forms, and treatment options.
What is Psoriatic Arthritis?
Psoriatic arthritis is a kind of inflammatory arthritis. It typically affects individuals who have psoriasis or a family history of the condition.
Arthritis is a chronic inflammatory condition that damages the joints – causing inflammation and pain (in and near joints). Psoriasis causes skin rashes and inflammation. Together, arthritis and psoriasis tend to affect both – skin and joints.
A telltale sign of PsA is patches of discoloured and flaky skin. These thick flakes or scales are known as plaques. This condition can also make your toenails and fingernails thick, scaly, and pitted (having small indentations).
The impact of PsA, however, is not limited to just skin, joints, and nails; this chronic autoimmune condition can also have negative impacts on the eyes, tendons, spine, gut, and even the heart.
Psoriatic Arthritis Symptoms
Psoriatic arthritis symptoms typically come and go episodically, in periods known as flares. Some common signs of PsA include:
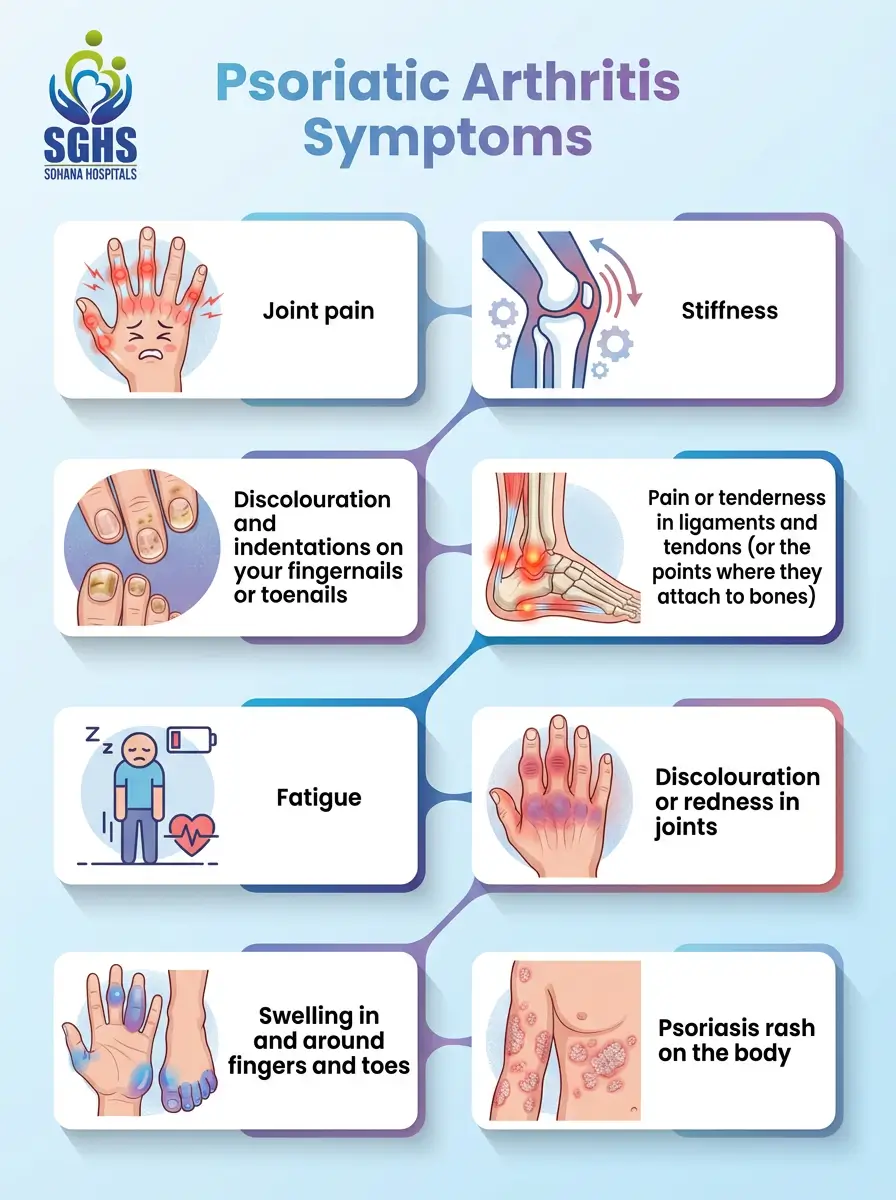
- Joint pain
- Stiffness
- Pain or tenderness in ligaments and tendons (or the points where they attach to bones)
- Discolouration or redness in joints
- Psoriasis rash on the body
- Swelling in and around fingers and toes
- Fatigue
- Discolouration and indentations on your fingernails or toenails
Psoriatic Arthritis Causes
There is no confirmed cause of psoriatic arthritis. While some surveys have revealed that people with PsA typically share the same genetic mutations, experts refrain from claiming that these changes in the genes are the sole or primary cause of the condition.
Besides that, around 40% of the individuals affected by PsA have a family history of the condition. This also points to it being a hereditary condition – passed down through biological generations.
Psoriatic Arthritis Forms
A specialist might categorise your psoriatic arthritis into one of the five forms of the condition. The forms are as follows:
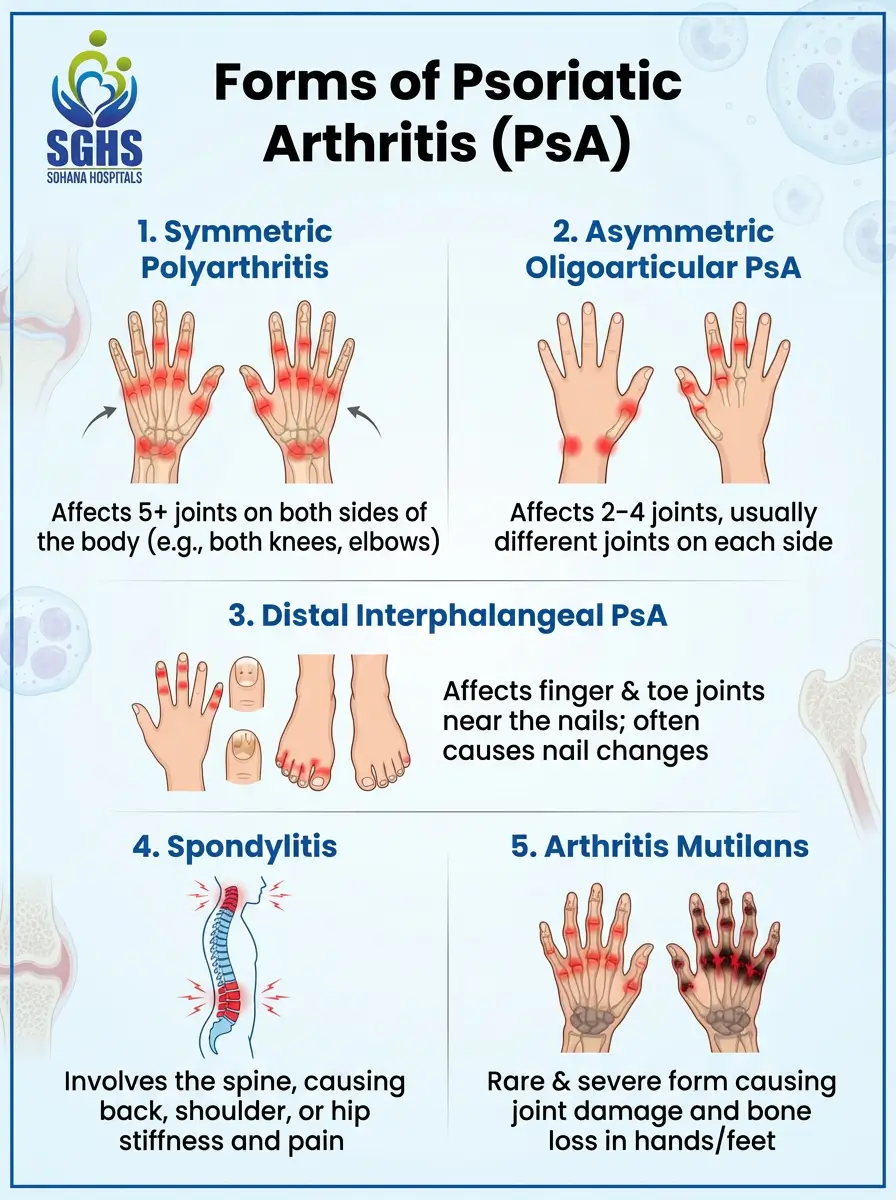
- Symmetric polyarthritis: This is one of the most common types of PsA. Polyarthritis is a form of arthritis in which 5 or more joints are affected at the same time. Symmetric polyarthritis tends to affect the same joints on both sides of the body. For instance: both elbows, both knees.
- Asymmetric oligoarticular psoriatic arthritis: This form affects two or four joints on both sides of the body. For instance: one elbow and one knee.
- Distal interphalangeal predominant arthritis: In this form of PsA, the joints near the tips of your toes and fingers (phalanges) are affected. This condition might cause your nails to look flaky, scaly, pitted, and discoloured.
- Spondylitis: In this type of PsA, patients experience inflammation and pain in the joints between the vertebrae (the 33 bones that make up the spine). This can also lead to pain and stiffness in the shoulders and hips.
- Arthritis mutilans: This type of PsA causes chronic symptoms in the hands and feet. The inflammation caused is typically chronic enough to lead to bone loss (also known as osteolysis). This is the rarest form of PsA.
Psoriatic Arthritis Treatment
While medical science has yet to find a permanent cure for psoriatic arthritis, there have been significant advancements in the field of PsA management. Here are a few treatment options your doctor might use to effectively manage your PsA symptoms:
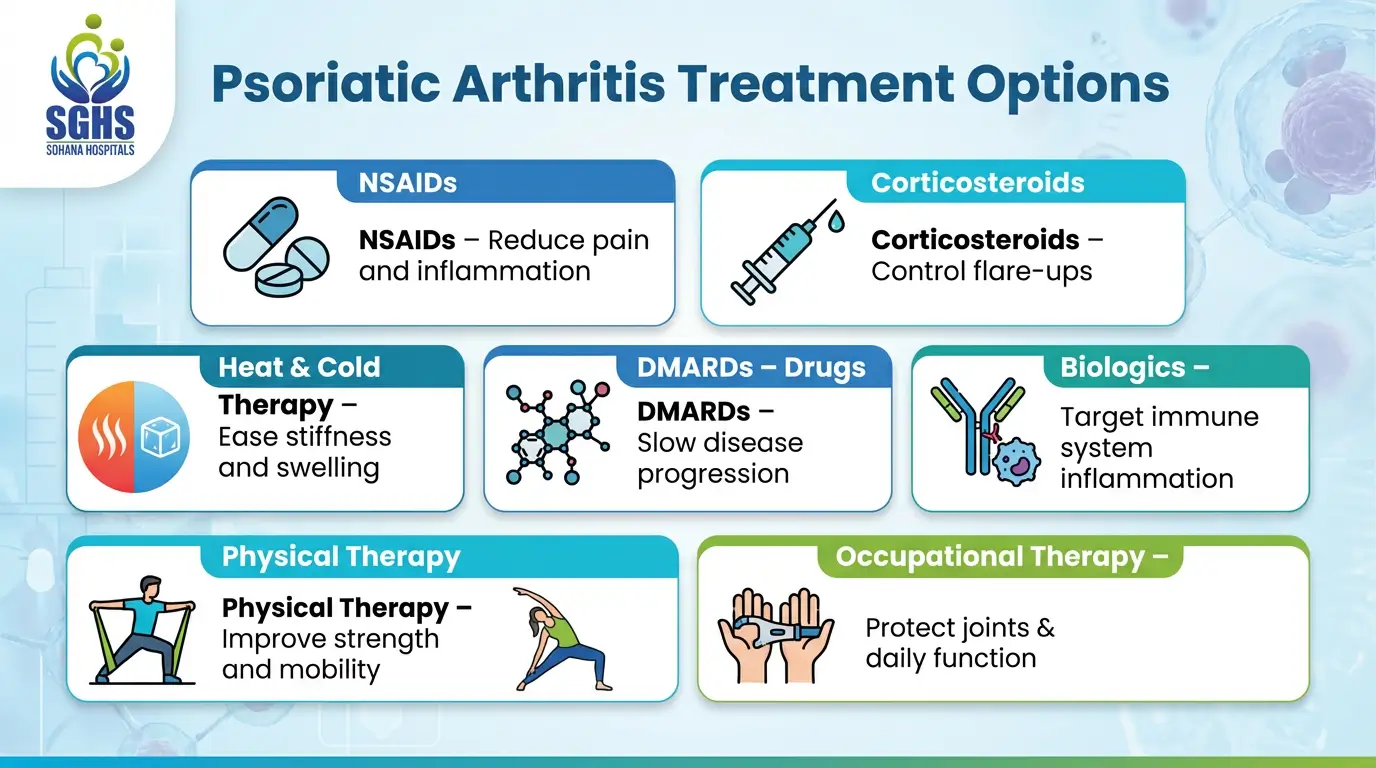
- Over-the-counter anti-inflammatory medication – NSAIDs
- Corticosteroids
- Heat and cold therapy
- Disease-modifying antirheumatic drugs or DMARDs
- Biologics
- Physical therapy
- Occupational therapy
When to Visit a Doctor?
30-50 years is when most PsA patients begin noticing symptoms. If you have a strong family history of the condition, you are advised to consult a specialist for screening or as soon as you notice the first sign. Early detection of the condition can lead to timely and effective management – giving you a pain-free, asymptomatic life.
If you book a consultation at Sohana Hospital, you can meet the best rheumatologist in Chandigarh and get started on your healing journey today! As a matter of fact, Sohana Hospital is one of the very few institutions in the tricity to have a dedicated rheumatology department treating hundreds of rheumatic patients every day.
Comprehensive diagnostic tests, modern treatment options, and a highly skilled team of specialists come together to give you the best psoriatic arthritis treatment in the tricity.
Frequently Asked Questions
1. Is there a cure for psoriatic arthritis?
No, there is no cure for psoriatic arthritis. However, modern medicine has advanced enough to manage and control the condition effectively, even helping many individuals become asymptomatic. The key is early detection. Visit a rheumatology doctor as soon as you experience symptoms and get started on your psoriatic arthritis management journey for a pain-free life.
2. What are the early signs of psoriatic arthritis?
Some early signs include joint pain, stiffness, flaky skin, scaly and pitted nails (fingers and toes), and inflammation around joints, etc.
3. What is the difference between rheumatoid arthritis and psoriatic arthritis?
Both rheumatoid and psoriatic arthritis are autoimmune conditions. However, their key differences are: RA usually presents symmetrically on both sides of the body and primarily affects only the joints. PsA, on the other hand, is not always symmetric and affects joints, skin, and nails.
4. How to treat psoriatic arthritis?
There are many ways to effectively manage psoriatic arthritis. Some common modes of treatment include: cold/heat therapy, NSAIDs, DMARDs, biologics, corticosteroids, physiotherapy, etc.
5. How is psoriatic arthritis diagnosis done?
There are many advanced diagnostic tools that help detect PsA. These include: X-rays, MRI, CT scan, blood tests, ultrasound, etc. It is important to note that autoimmune diseases can be a little difficult to detect in the initial stages. So, if you have a family history of the condition, the key to effective management is regular screening.
Reference Source:
